Billing Services for your Large Practices
Save up to 30-60%
Billing inaccuracies can ruin your large practices financial growth. Over ten years, Med Revolve Billing has been able to mitigate lost revenue and bring down denial rates for larger practices by 98%.
THAT OUR SERVICES PROVIDE
BENEFITS

Faster and More Cash Inflow

Billing and Coding Accuracy

Improve Patient Experience

End-to-End Denial Management

Compliance Regulation

Cost Savings
Rock-solid billing, faster payments
Hospitals face these difficulties, such as patient registration, claims submission and follow-up. The major struggle is filing numerous claims apart from other administrative burdens.
An effective billing infrastructure ensures transparent, affordable and flexible solutions that can fill gaps in the procedures of billing. Advanced systems manage company’s billing services – with denial management tools in place and competent teams – to deliver remedies and round-the-clock supports.
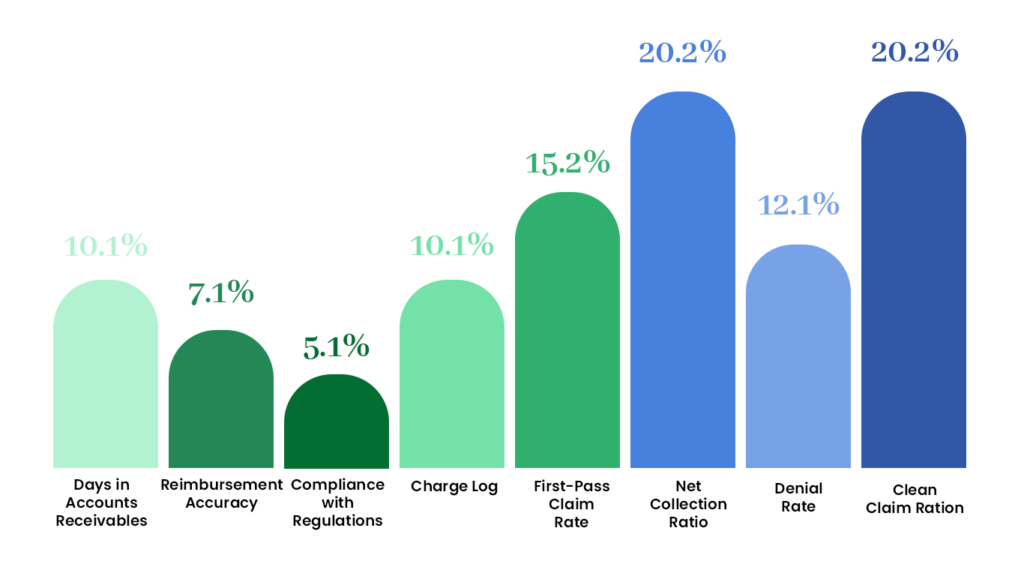
8 Important KPIs to Ensure Faster and More ROI
These metrics make up most of the revenue cycle management flowchart for the billing process and revenue cycle management of your large practice.
We employ four key metrics to audit billing and optimize ROI for your large practices
Efficiency, productivity, and financial performance are the three parameters that make up 60% of your billing process.
Our clients have first-hand experience to support these figures.
Days in Account Receivables 30-40 days:
Our process for managing receivables involves taking into account the normal number of days it generally takes the company to recover outstanding debts. By reducing the accounts receivable days ratio, we guarantee faster repayment.
The First Pass Rate of Acceptance - 97%
Another term for the first pass acceptance rate is clean claim rate, this is the percentage of claims that they approve it at the very first time. Our excellence in top management of revenue cycle services has led us to an unprecedented first-pass clean claim rate of 97%, which truly demonstrates our commitment to quality.
Overall payment rate - 98%.
The overall collection rate is 98 percent, considering both the collections from patients and insurance. We have a continuously high net collection percentage of 98% and we promise prompt payment receipt at all times.
Denial Rate - 1%
Proportion of claims can measure efficiency of your revenue cycle control approach. We follow up denied claims, scan and correct inaccuracies, and increase income production.
Get Medical Billing Services to Refine your Billing, Coding, and Overall RCM Strengths
Recognizing the fact that one size doesn’t fit all, we provide customized services to meet the unique needs of your large practice with transparent and mistake-free processes. Our overall approach includes evaluation of your billing procedure, identification and rectification of issues, as well as management of unpaid and overdue insurance claims.
If you have a large practice, and non-clinical stress is bothering you because of problems such as registering patients, claims filing or rejection management, we are there to help out. We will enable you to provide quality patient care through our actions.
It is true that we make sure that more than 99% of our claims are clean, submit medical claims promptly, do daily follow ups on aging A/R and raise the level of reimbursement.

Medical Billing Services to Streamline Revenue
Cycle Management for Large Practices
To simplify the intricacies of medical billing and improve your financial and healthcare output,
choose the subsequent billing flowchart for your big firm.

Insurance Verification and Eligibility
Ensure prior authorization and verify insurance eligibility for medical services such as diagnoses, procedures, and treatments

Patient Registration
Collect, verify, and enter the data into the system to ensure accuracy and error-free billing documentation.

Claims Submission
With a 99% clean claim rate we submit accurate claims to ensure a high first-time pass rate so you get the maximum collection rate.

Coding And Documentation
We deploy expert coders and billers to prevent errors and inaccuracies in diagnostic and procedural coding

Denial Management
Collect, verify, and enter the data into the system to ensure accuracy and error-free billing documentation.

Payment Posting
With a 99% clean claim rate we submit accurate claims to ensure a high first-time pass rate so you get the maximum collection rate.

A/R Follow Up
We follow-up on pending payments and accounts receivables for reimbursements and remaining collections.

Patient Billing
Patients are billed with accurate charges to cover their bills against the services they have availed.

Education And Outreach
By proactively engaging with providers, we help to understand patient's financial obligations and encourage timely payments.
01
24/7 Access to Technology and Infrastructure
Efficiently supports operations and personalizes billing and RCM for large practices are advanced billing technology, coding tools, and infrastructure. By outsourcing your billing to Med Revolve Billing, you can leverage these technological resources without incurring costs on software or hardware.


02
Regular Auditing and Quality Control
The regular internal audits ensure that the billing processes are free from errors and provide opportunities for improvement. Additionally, we rectify these patterns and institute some quality control measures like checking claims twice and conducting reviews. This helps in reducing revenue gaps and inaccuracies.
03
Upfront Communication
Long-term work partnerships require clear and effective communication among insurers, administrative staff and billing personnel. This builds trust between the parties involved as well as minimizing any misunderstandings or errors that may occur.


04
Expertise and Specialization
Fewer denials are ensured through experience and professionalism. Our coding, billing, and claims submission team is composed of professionals who are experts in this field. For your large practice to achieve compliant billing practices, you can exploit the expertise that we have.
05
Simplifying Complex Coding System (ICD-10, CPT, HCPCS)
Our firm is constantly updated to meet the new codes, rules and regulations of diagnostic coding, as well as insurance requirements. The company has coders who have experience in ICD-10, CPT and HCPCS codes for diagnostic procedures; thus making it efficient in terms of accuracy and quick collection.








