Medical Coding Services
Best Medical Coding Solutions, No Financial Bleeding
Medical coding services are essential for healthcare providers. Our expert panel of coders provides the best medical coding solutions. Moreover, it fulfills the coding needs of every specialty by assigning diagnosis and procedure codes and facilitating the creation of claims for submission to payers.
- Providers receive timely payment.
- Patients are accurately billed for services.
- Payers accept claims without rejection.
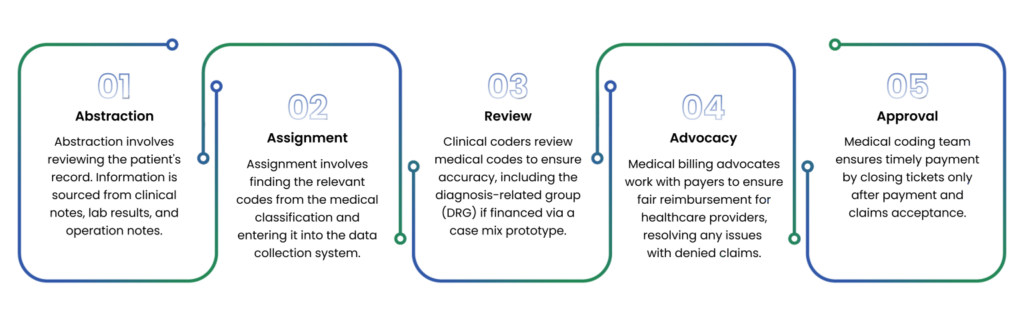
What Do Our Coders Do?
Practice Documentation Analysis
Our coders carefully analyze medical documentation that healthcare provider provides. Moreover ,they classify this information using standardized CPT codes.
Medical Diagnosis Coding
Our coders convert diagnosis procedures into codes that insurance companies can easily read and that are hassle-free for medical providers.
Claim Submission
Our coders work with the billing team to generate a super bill that includes charges the payer is responsible for patient insurance coverage, and any co-payments.
Claim Approval
Our coders advocate for the healthcare provider to ensure the claim is approved. Furthermore, they work to recover Aged Receivables and help ensure that denied claims are paid.

Medical Coding Experts
Accurate medical coding has become a necessity; particularly, since the ACA law has obligated healthcare providers to furnish patients with medical services they receive, along with their corresponding expenses.
Inaccurate coding leads to claim denials, resulting in revenue shortfalls for the provider. In addition, unintentional fraud can occur through unbundling, causing patients to be overcharged for services. Furthermore, there are growing complexities in legislative mandates.
Med Revolve billing – a best medical Billing Agency – company offers the best medical coding services. Moreover, our certified medical coders are highly trained in advanced coding techniques to accurately code the services provided to patients. Ultimately, we ensure providers receive fast and accurate reimbursements without any claim denials.
Complete Medical Solution Provider
One Solution for All Your Medical Coding Needs
Med Revolve Billing – a best medical billing agency -handles all the complex aspects of medical coding, such as assigning accurate and compliant
codes for various specialties, procedures, and diagnoses. The important thing is that we optimize your revenue cycle and focus on key metrics and indicators, such as:
- Managing Overlook for Coding (OFC)
- Calculating Risk Adjustment Factor (RAF) Score
- Improving Discharged Not Final Billed (DNFB) Rate
- Managing Discharged Not Finally Coded (DNFC) Cases
- Optimizing Diagnosis-Related Group (DRG)
- Increasing Case Mix Index (CMI)
Managing Overlook for Coding (OFC)
This is a proprietary algorithm that we use to measure and manage the productivity and quality of our coding team. It allows us to monitor the coding process in real-time, identify and correct errors, and generate reports and analytics.
Calculating Risk Adjustment Factor (RAF) Score
This is a measure of the expected health care costs for a patient based on their diagnoses and demographic factors. A higher RAF score indicates a higher risk and complexity of the patient’s condition. We use our expertise in coding and documentation to ensure that your RAF scores accurately reflect the severity of your patient population and maximize your reimbursement from Medicare Advantage plans.
Improving Discharged Not Final Billed (DNFB) Rate
This is a proprietary algorithm that we use to measure and manage the productivity and quality of our coding team. It allows us to monitor the coding process in real-time, identify and correct errors, furthermore generate reports and analytics.
Managing Discharged not Finally Coded (DNFC) Cases
This is the number of days a case remains before being finally coded after discharge. A high DNFC can delay your claim submission and reimbursement, as well as increase your coding backlog and workload. We help you lower your DNFC by providing fast and accurate coding services, using our OFC software and our skilled coders.
Optimizing Diagnosis REALTED Group (DRG)
This is a system that classifies hospital cases into groups that have similar clinical characteristics and resource use. Each DRG has a relative weight that reflects the average cost of treating a patient in that group. DRGs are used by Medicare and other payers to determine the payment rates for inpatient hospital services. We help you optimize your DRG assignment by applying our knowledge of the MS-DRG system, the coding rules, furthermore the documentation requirements.
Increasing Case Mix Index (CMI)
This is the average relative weight of the diagnosis-related groups (DRGs) for all patients treated at your facility. A higher CMI indicates that you have treated more complex and resource-intensive patients, which may result in higher reimbursement rates from Medicare and other payers. We help you improve your CMI by assigning the most appropriate DRGs for your cases, based on the ICD-10-CM and PCS codes and the MS-DRG system.

Are You Frustrated with Medical Coding Errors, Denials, and Delays?
Med Revolve Billing – a best medical billing agency – provides complete medical coding solutions and services. Furthermore, our certified coders handle all coding projects — in patient, outpatient, emergency, or specialty services. So, don’t let medical coding problems affect your bottom line; our experts will detect and correct them before they damage your practice.
Expert Medical Coders and Billers
Facility Coding Service
Facility coding involves coding the services that a healthcare facility provides to an inpatient, such as the use of a wheelchair, hospital room, and moreover nursing care. Moreover, our facility coders use their HCPCS coding knowledge to accurately code the facility’s services and then help the facility receive the correct reimbursement.
Professional Fee Coding Service
In professional fee coding, also known as ProFee coding, doctors assign codes to patient checkups and treatment services. Furthermore, Our experienced professional fee coders accurately translate a physician’s services into billable codes, ensuring that the physician is fairly compensated by the payer and the patient is billed correctly for the services they received.
Payer Specific Coding Service
Different payers have their own coding guidelines, which makes the physician coding process more challenging. Our coders are well-versed in the coding guidelines of all major payers in the US, including UnitedHealth Group and Cigna, and Humana. Also, our medical coders have developed payer-specific Local Coverage Determination (LCD) guidelines to ensure coding accuracy for physicians.
Offshore Coding Service
Offshore coding is the process of hiring coding professionals in other countries to perform best medical coding tasks. This is a cost-effective way to obtain high-quality coding services, as wages in other countries are frequently lower than in the United States. We provide offshore coders for any healthcare organization, while guaranteeing HIPAA compliance
General Practitioner Visits Coding Service
General Practitioner Visits Coding is a process that assigns codes to medical procedures and diagnoses for billing purposes. Our expert physician coders can handle this task with ease and accuracy. Moreover, we make sure that practitioners receive accurate reimbursements and claim approvals, which can be beneficial for their practice.
Outpatient Coding Service
Outpatient coding is a medical coding process used for patients who receive treatment but are not admitted to the hospital for an extended stay. Our medical coders are proficient in the latest documentation guidelines for outpatient evaluation and management (E/M) visit codes. They also accurately use ICD-10-CM and HCPCS codes for smooth cash flow at the healthcare organization.
HCC Coding Service
Hierarchical condition category (HCC) coding is a specialized field that relies on a risk-adjustment prediction model and is linked to over 10,000 ICD-10 diagnosis codes. Our trained HCC coders are experts in the regulations surrounding this risk adjustment model and use their expertise to ensure that diagnosis codes have assigned RAF scores for both commercial risk adjustment and Medicare Advantage risk adjustment.
Inpatient Coding Service
Inpatient coding is used for patients who require hospitalization and must be admitted for an extended stay. Our coders are certified with the Certified Inpatient Coder (CIC) credential, which validates mastery in abstracting information from the medical record for ICD-10-CM and ICD-10-PCS coding. We also have experience with Medicare Severity Diagnosis Related Groups (MS-DRGs) and the Inpatient Prospective Payment System (IPPS). This optimizes the revenue cycle of a provider by reducing claim denials and ensuring timely payments.
Data Security
Keeping Patient Data Safe
Med Revolve Billing – a best medical Billing Agency – is a medical coding solutions provider that values the security and confidentiality of your patient data. That is why we adhere to the HIPAA standards and use the latest encryption, firewall, antivirus, and other security technologies to protect patient’s data from any unauthorized access, use, or disclosure

Compilance And Hippa
Compliance in Medical Coding Solutions
Our Medical Coding Solutions follow the HIPAA Privacy Rule and the HIPAA Security Rule for the collection, storage, transmission, and disposal of protected health information (PHI). We comply with all the US government healthcare data regulations, such as Medicare Access, the Merit-based Incentive Payment System (MIPS), the Medicare Shared Savings Program (MSSP), the Comprehensive Primary Care Plus (CPC+), and a lot more.
Best Medical Coding Company
Why Choose Med Revolve Biling for Medical Coding Services?
Choosing the best medical coding company for your medical coding services is a crucial decision that can affect your revenue cycle along your compliance. Here are some reasons why you should choose Med Revolve Billing – a best medical billing agency- medical coding company as your medical coding solutions provider:

Staffing Requirements
Finding, training, and retaining medical coders can be costly. By outsourcing your medical coding to us, you can eliminate these hassles and focus on your core business. We have a team of AHIMA and AAPC certified coders who can handle any specialty and volume of work

Denial Assistance
Finding, training, and retaining medical coders can be costly. By outsourcing your medical coding to us, you can eliminate these hassles and focus on your core business. We have a team of AHIMA and AAPC-certified coders who can handle any specialty and volume of work.
Specialty Specific
By using our excellent medical coding services, there’s a reduction in denial rate and an increase in revenue. We use modern medical coding solutions to detect and correct coding errors before claim submission. Our experts appeal to any denied claims by providing supporting evidence.

Complete Auditing
Nephrology, radiology, orthopedics, and pediatrics have complex codes that require specific expertise. By choosing our medical coding company, physicians can benefit from our specialty-specific coding services. Our nosologists can assign compliant codes for every medical case.

Staying Compliant
Medical coding is constantly affected by regulatory changes. These changes include new codes, deleted codes, revised codes, updated guidelines, or modified policies. By using our medical coding solutions, your practice stays updated with the latest regulatory changes.
Backlog and DNFB
Backlog refers to the number of cases pending to be coded after discharge. DNFB refers to the ratio of accounts that are not final billed due to incomplete or inaccurate coding or documentation. Our 5-star medical coding services clear your backlog and reduce your DNFB.
Don't Let Medical Coding Errors Cost You Your Revenue.
Med Revolve Billing’s Medical Coders Are Here To Serve You!
Med Revolve Billing – a best medical billing agency – offers the best solutions for all medical coding challenges. Our clinical coders gracefully handle any specialty and volume of coding. We use the latest EHR technology to ensure compliance. We also provide physicians with transparent reports to monitor their coding performance and revenue cycle.